 Megan McArdle spoke on antibiotic resistance at the Economic Bloggers Forum yesterday. McArdle is a journalists who writes for the The Atlantic, primarily on economics, finance, and government policy.
Megan McArdle spoke on antibiotic resistance at the Economic Bloggers Forum yesterday. McArdle is a journalists who writes for the The Atlantic, primarily on economics, finance, and government policy.
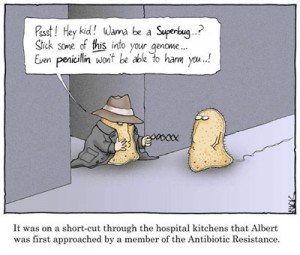
Her presentation, “Antibiotics: The world’s most broken market,” was interesting. Notice (in the video below) that she never questions the market-driven premise of pharmaceuticals – and by extension, the for-profit nature of medicine and health care. That’s not her politica/economic persuasion.
Here’s an excerpt from the talk where she discusses the patient/doctor end of the antibiotic resistance problem. What she says is already quite familiar. What’s interesting is her frank description of how doctors behave and how patients in turn regard doctors.
People love to get antibiotics. They go to their doctor and they’re like, “My kid has an earache. Give him antibiotics.” Now the doctor could say, “No we shouldn’t. We should wait and find out if it’s bacterial. Almost all ear infections are bacterial. Due to throat infections. Due to almost anything you can name. But to do that, the doctor has to sit down and deal with an angry patient who may pick up and leave their practice.
If you look at the way that the current insurance industry is organized, right, what do doctors need? They need volume. They get paid by volume. Reimbursements for primary care physicians, who are where a lot – by no means all – but where a lot these vaccines go through, are very low. They’ve made up for that, and you all know this, right. You go into your doctor, and the minute you start talking, your doctor exudes an almost visible — like — desire for you to leave now. So that they can go on to the next patient. So what do they do? They give antibiotics to patients to shut them up. It takes too much time to explain and the risk of losing the patient is high.












